Things to consider when taking a biologic

Biologics are a type of medication that can be prescribed for some forms of inflammatory arthritis including rheumatoid arthritis (RA).
This resource gives you general information about how biologics work, why they are used, as well as tips on the safe use of these medications.
This resource does not provide advice about the specific biologic you may be prescribed to manage your RA. It does not cover all the side effects and safety precautions that can occur with each biologic. You should discuss this with your doctor, rheumatology nurse or pharmacist, or see the For more information section at the end of this resource.
What is a biologic?
Biologics are medications that can be used to treat certain types of arthritis including RA. They are a type of medication called a disease-modifying anti-rheumatic drug or DMARD for short which may prevent the development of joint damage. DMARDs, including biologics, are different to medicines that simply block the pain or other symptoms you’re feeling. They work by blocking specific substances in the immune system.
Usually the immune system fights infections to keep you healthy. In autoimmune diseases such as rheumatoid arthritis, the immune system mistakenly takes aim at itself, attacking its own healthy tissues. This leads to very high levels of certain natural substances, called cytokines, in the body that then cause joint inflammation and pain. Biologics are very effective at blocking these substances. This dampens down the immune system, and reduces inflammation, pain and damage to the joint.
Biologics mimic substances naturally produced by the body. They are made from living cells, which is the key difference from most other medicines that are made from man-made or chemical compounds. They can be very effective in treating RA and tend to work more quickly than conventional DMARDs (eg. methotrexate). There are a number of biologics that target different parts of the immune system. If your RA does not respond to one type of biologic, your rheumatologist (arthritis specialist) may use a different biologic to see if it works better for you.
Biologics can also be used in combination with other conventional DMARDs, particularly methotrexate. The combined treatments may be more effective than the individual medications in some cases. Talk to your rheumatologist or rheumatology nurse to better understand the pros and cons of using a combination of a biologic and a DMARD.
When are biologics used as a treatment for arthritis?
Biologics are not routinely prescribed for all people with RA. They can only be prescribed by a specialist, such as a rheumatologist, and under strict criteria. They are usually only given to people whose RA has not adequately responded to conventional DMARDs or who have had side effects from them. The decision to prescribe biologics is not made lightly and it is normal to need time to consider the pros and cons of using this type of medication. Work with your rheumatologist and rheumatology nurse to understand why biologics have been recommended and communicate any concerns or fears you might have so that they can support you to make the best decision.
Types of biologics
There are currently five different types of biologics available. Each targets a different part of the immune system to help reduce inflammation and joint damage. These are:
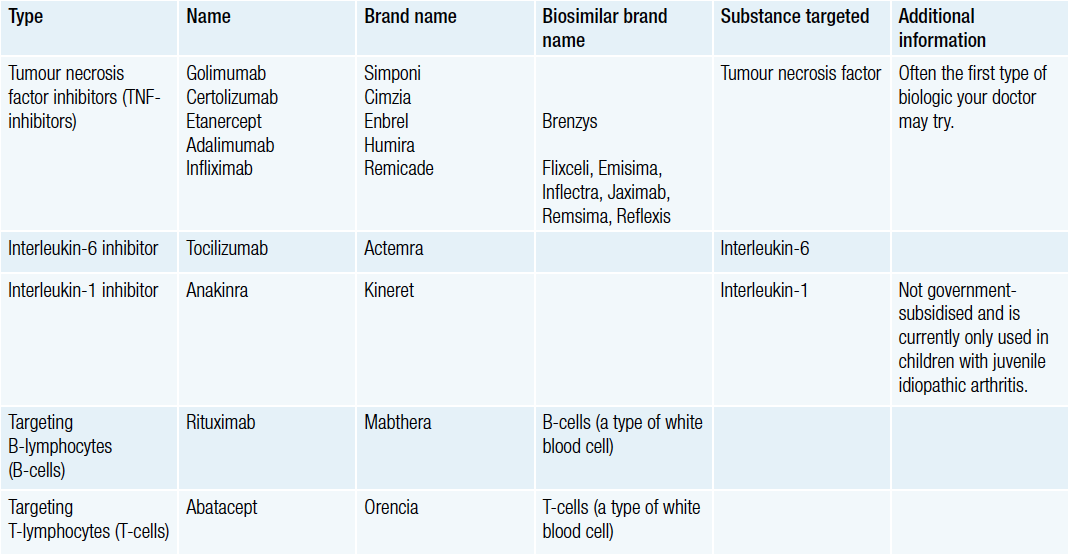
Biosimilars
For some biologics, there may be a biosimilar medication available. A biosimilar medicine is a copy of a biologic medicine that has been shown to be highly similar to the original medicine.
The nature of biologics means they cannot be copied exactly. Biologic medicines are complex and are produced using living cells so there are minor differences between brands and batches. This is why competitor brands are called biosimilars as they are highly similar but not exactly the same.
Biosimilar medicines are comprehensively tested to establish that they have similar safety and effectiveness as the original biologic. However, as they are not identical to the original biologic, switching to a biosimilar may not be the right decision in every case, especially if the original biologic is working well for you.
It is important that you and your rheumatologist decide together whether you should keep taking the same medication or whether you could consider a biosimilar. If your rheumatologist wants you to continue with the original medication, they will tick the non-substitute box on your prescription. If the pharmacist asks whether you want to consider a substitution, request the medication that is on the script and not a substitution. Further information about biosimilars is available at www.arthritisaustralia.com.au
How are biologics given?
Most biologics are given as either an infusion (a drip into a vein) or an injection via a needle. Infusions are usually given by a nurse at a hospital or clinic, or sometimes at home. Injections are given via a needle, usually into the stomach area or thigh. Your rheumatologist, rheumatology nurse or pharmacist will usually teach you how to safely do the injection yourself, or teach a trusted friend or family member to do it for you. Alternatively, your GP or their nurse may be able to do the injections for you.
How often do I take the biologic?
Each biologic has its own schedule or frequency of when it is given. Depending on which biologic you are using, you might need to take it daily, weekly, fortnightly, monthly or only a few times per year. Make sure you have a clear understanding from your rheumatologist or rheumatology nurse of how often you need to take your medication so there is no risk of missing a dose or taking too much. As with any medication, it can only be effective if you take it as directed.
TIP: Taking a medication once a week, fortnightly or monthly can be difficult to remember. Write it in your diary or set an alarm or reminder in your phone/computer to remind you when to take your next dose.
Before starting a biologic
Before a biologic is prescribed, your rheumatologist will typically talk to you about the following:
- Infections. If you have an infection or have a history of chronic (long-term) infection, your doctor will not start you with a biologic until the infection has been treated.
- History of tuberculosis (TB), hepatitis B or hepatitis C. Biologics can cause certain bacterial or viral infections to reactivate. Your rheumatologist will often recommend tests for TB and hepatitis before starting a biologic.
- Live virus vaccines. Talk to your doctor about your immunisation status and whether any vaccinations are recommended. Any live virus vaccine needs to be given one to three months before starting a biologic. (see Vaccinations below)
- Other vaccines. Your doctor will usually recommend certain vaccines, such as the flu vaccine, pneumovax and Hep B, before starting treatment.
- Future surgery. Treatment with a biologic may be postponed if you are planning on having surgery.
- Smoking. It is recommended to stop smoking while you are taking a biologic.
- Latex allergy. Let your doctor know if you have an allergy to latex as some of the equipment used to inject certain biologics may contain latex. Most companies are also releasing latex-free products which may be more suitable.
Safety
Biologics can be positively life-changing medications for people with RA. They are very effective in dampening the immune system and inflammation. However, the immune system also has an important role in protecting you from infections and illness. Your rheumatologist will aim to find the biologic and the dose that allows you to achieve a balance between the risk of side effects and controlling the arthritis.
Infections
One of the unwanted effects of using a biologic is an increased risk of infection. You may experience mild infections, such as colds and sinusitis, more often than usual. These minor infections may also last longer than normal. More importantly, the minor infections can lead to more serious infections such as pneumonia. Your doctor or rheumatology nurse will advise you which symptoms of infection are mild and do not need medical treatment, and which are more serious and require immediate medical attention. They will also tell you who to contact if you are unwell if your GP or rheumatologist are not available. You can reduce your risk of getting an infection by avoiding close contact with people with active infections and by having the appropriate vaccinations.
Vaccinations
You should not have any live-virus vaccines if you are taking a biologic. These include:
- Shingles (herpes zoster) vaccine
- MMR (measles, mumps and rubella) vaccine
- OPV (oral polio vaccine)
- BCG (Bacillus Calmette Guerin) vaccine
- Some travel vaccines, such as typhoid, small pox and yellow fever vaccines.
Inactivated (dead or killed) vaccines, such as pneumovax and the yearly flu vaccination, are safe and recommended to reduce your risk of those infections. Ask your doctor about which vaccinations are recommended while taking a biologic and always talk with your doctor before receiving any vaccinations.
Cancer risk
The substances blocked by biologics may also play a role in the body’s defence against cancer. There have been concerns that blocking these substances may result in a higher chance of developing cancer. However, over the many years of using and studying biologics, there have been isolated reports of cancer but no firm or consistent evidence of a greater risk of cancer than would have been expected.
Some types of cancer are more common in people with severe active inflammatory arthritis, such as lymphoma (cancer of the lymph glands). However, treatment with biologics does not appear to increase this risk further.
For general cancer prevention, stop smoking, have regular skin checks with your GP or a specialist, protect your skin from the sun, maintain a healthy body weight, limit alcohol intake and eat a healthy, balanced diet.
Pregnancy and breastfeeding
Before you try to conceive, it’s important to speak with your rheumatologist about all your arthritis medications, including biologics. Some medications are not recommended to be used during pregnancy, while others may be continued throughout or for part of the pregnancy. Some medications can stay in the body for a period of time after you stop taking them so you may need to stop them a few months before you try to conceive. Some medications are safe to take while you are breastfeeding while others should not be used. If you are thinking of becoming pregnant in the near future or are not using contraception, you should discuss the most appropriate treatment options with your rheumatologist or rheumatology nurse.
If you fall pregnant unexpectedly, contact your rheumatologist immediately for advice.
Travel
You can still travel domestically and overseas while taking a biologic but plan ahead. Talk to your rheumatologist to ensure you have an adequate supply of your biologic to last your trip, as well as advice on managing your medications while travelling. For example, ensure your medications are in your hand luggage with a letter from your doctor. Talk to your rheumatologist about any vaccinations you may need before your trip.
CONTACT YOUR LOCAL ARTHRITIS OFFICE FOR MORE INFORMATION AND SUPPORT SERVICES