Already pregnant or just starting to think about pregnancy? Becoming a parent is one of the most exciting and overwhelming times in most people’s lives. But even more so if you, or your partner, has arthritis.
I have arthritis…is having a family possible?
Absolutely. It might require extra planning and patience, or not be quite as you pictured it, but becoming a parent is usually possible if you have arthritis.
The journey to parenthood can be uncertain and demanding, often both physically and emotionally, and sometimes more so if you are living with arthritis. Living with joint pain and other symptoms can make it challenging to care for a new baby or an active toddler. However, with proper planning and medical care, most people with arthritis can have safe, successful pregnancies and become loving, capable parents.
The first step on the path towards parenthood is to discuss your family plans with your rheumatology team before you start trying for a baby
Does having arthritis make it harder to fall pregnant?
Conceiving a baby may take longer if you, or your partner, have arthritis but experts are not exactly sure how or why. Studies have shown that women with rheumatoid arthritis do take longer to conceive, often longer than 12 months. Experts aren’t sure why this is the case. It could be due to the disease itself or some arthritis medications, such as anti-inflammatory medications. Other factors such as lower sex drive due to fatigue and pain might also play a role.
It is estimated that as many as one in six couples in the Australian population have trouble conceiving, so if this is an issue for you, you are definitely not alone. The good news is that advances in medicine and science have made treatments for fertility challenges more effective.
If you have any concerns about your fertility, speak to your GP or rheumatologist who can refer you to a fertility specialist, such as an obstetrician, to improve your chances of getting pregnant. It can be a lonely, emotionally draining experience if it’s taking longer than you had hoped to fall pregnant, especially if you have ceased some of your medications in order to conceive safely.
Is there an increased risk of miscarriage or problems during pregnancy if I have arthritis?
Most studies have found that the rates of miscarriage for women with rheumatoid arthritis are no different from rates for women without arthritis.
There is also no increased risk of miscarriage if the father has arthritis. Most types of arthritis that are well controlled don’t increase the risk of complications during pregnancy or cause harm to the unborn baby.
Highly active, or poorly controlled, arthritis can cause risks for both you and your unborn baby, so it is vital to work with your rheumatology team to find a management plan that works for you.
Can arthritis be passed on to my unborn baby?
For most types of arthritis, the chance of your child having arthritis is low. Even though some types of arthritis appear to run in families, there are many other factors involved other than just the genes your baby inherits from you and your partner.
If you are worried, it’s a good idea to talk to your rheumatologist for more specific information about your particular type of arthritis.
We want to start a family – what do I need to consider?
Get the right advice – see your rheumatologist before planning for a baby. Some of the medications used to treat arthritis can be taken safely before and throughout pregnancy. Some can be used at certain times during pregnancy. Others are harmful to a growing baby so shouldn’t be used during pregnancy. Some medications remain in your body for many months after you stop taking them so you may need to wait a while before trying to conceive.
If you or your partner has arthritis, make it a priority to talk to your rheumatologist at least six months before you start trying to conceive.
Your rheumatologist can give you advice about the safest combination of medicines to continue taking during conception and pregnancy, other treatments you could use while trying to conceive, and which medicines should be stopped before conception (and when you should stop them).
Suddenly stopping your medications could make your arthritis worse, which can cause health problems for both you and your baby. Always talk to your rheumatologist before you stop taking any of your arthritis medications. Remember, there are many arthritis medications that can be safely used before and during pregnancy.
Questions for your healthcare team
Here are some things to discuss with your healthcare team, such as your rheumatologist, rheumatology nurse and GP before you start trying to conceive:
1. Are there any medications in my treatment plan that I should stop taking while I’m trying to fall pregnant or when I am pregnant? If yes:
- How long should I stop taking the medication(s) before I start trying for a baby?
- What are my other options to help manage my symptoms while I can’t take my usual medication?
2. Are there any medications for arthritis that are safe to continue while I’m trying for a baby, and during pregnancy?
3. Do I need any vaccinations before trying for a baby, or if my medications are changing?
4. Should I be taking any supplements before trying to fall pregnant?
5. When would be the best time for my partner and I to start trying for a baby?
6. What is the best type of contraception we should be using while we’re waiting to conceive?
7. Are there any tests I need before trying to conceive?
Your medical team should be able to work with you to come up with a treatment plan that protects the health of your unborn baby, while also keeping your arthritis under control. Be mindful that treatment plans may need to change, or you may need to try a range of different medications to find the right treatment for you during this period.
If you find it hard to talk openly and honestly with your doctor about your options or concerns, write down your questions before the appointment. You can also consider seeking a second opinion from another rheumatologist with a special interest in pregnancy.
Does it matter how active my arthritis is before I conceive?
You might be eager to start a family, but your rheumatologist only wants to talk about how to get your arthritis under better control. Why does it matter whether your arthritis is active if you’re trying to conceive? Conceiving while your arthritis is not well controlled or highly active can cause risks for both you and your unborn baby.
Having your arthritis well controlled may:
- make it easier for you to conceive
- reduce your chance of requiring a caesarean section to deliver your baby
- reduce the chance of your baby being born prematurely, or having a low birth weight
- prevent permanent joint damage and disability to you.
It is vital to work with your rheumatology team to find a plan that works for you and puts you on the path to a healthy pregnancy and baby.
What about men with arthritis?
If you are a man with arthritis and you are thinking about starting a family, your medications could also affect your fertility or your unborn baby. Most medications can still be taken but some may need to be stopped, possibly for several months, before trying for a baby. Some medications can reduce your sperm count, although this is usually reversed when you stop taking them.
Talk to your rheumatologist at least six months before you and your partner plan to conceive.
Your rheumatologist can give you advice about the best treatment plan to follow before conceiving. Be vigilant with contraception to prevent unplanned pregnancies until you are ready to conceive.
When is the best time to start trying for a baby?
The best time to start trying for a baby is when your arthritis is well controlled or stable. While you might get a sense of this yourself from monitoring your own symptoms, it is important you discuss with your rheumatologist whether your arthritis is stable.
If your arthritis is not well controlled, you may find it harder to conceive and there can be risks for both you and your unborn baby. Talk to your rheumatologist about the best management plan that will give you the best chance of achieving your goal of becoming a parent while also protecting the health of you and your baby.
You may also need to wait after stopping certain medications; for example, methotrexate needs to be stopped at least three months before trying to conceive.
Stop smoking and avoid recreational drugs to reduce the risk of harm to your baby. Eat a healthy balanced diet, lose any extra body weight, start taking a folic acid supplement and lead a healthy lifestyle to further boost your chances of a healthy pregnancy.
What is the current evidence about medication safety for pregnancy and breastfeeding?
If you are planning a pregnancy it is vital to get an expert opinion from your rheumatologist about your medications as early as possible. Some arthritis medications are safe to continue before and during pregnancy. Other medications may need to be stopped as they may increase the risk of miscarriage or cause harm to a developing baby. Your rheumatologist will work with you to find the right arthritis management plan for both your health and the health of your unborn baby.
The current evidence about the safety of arthritis medications is summarised on the below table. This is a general guide only. New information is being discovered regularly and advice may be updated. Use this table to discuss your medications with your rheumatologist and always follow their expert advice.
Unplanned pregnancy
If you, or your partner, have fallen pregnant unexpectedly, call your rheumatologist or treating doctor immediately.
If you are taking any of the medications from the "Not safe" column in the table below, stop taking them as soon as you find out you are pregnant and contact your doctors.
If you are taking any of the medications from the "Generally safe" or "May be safe" columns in the table below, continue taking them as usual until you speak to your rheumatologist. Do not stop taking these medications without first talking to your rheumatologist and getting the right advice.
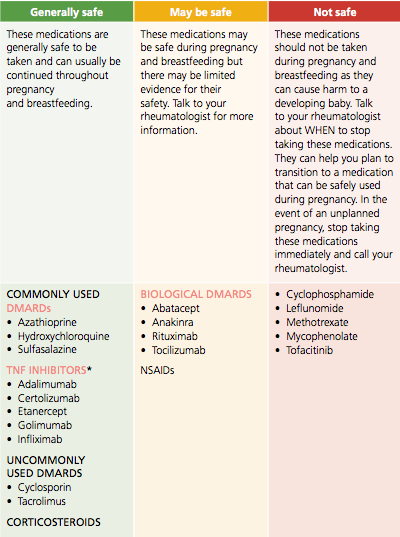
* Some TNF inhibitors are recommended to be stopped in the later parts of pregnancy. Talk to your rheumatologist for more information.
Pregnancy and arthritis – what can I expect when expecting
The day you’d been hoping for has arrived…you’ve had a positive pregnancy test and you are now taking your first steps towards parenthood. Congratulations!
How will I feel during pregnancy?
The greatest myth of pregnancy… the pregnancy glow!
How your body will respond to pregnancy, and how you will feel during the next nine months, will be different for everyone. Every woman is unique, and every woman’s pregnancy is also unique.
Some women sail through pregnancy and even find that that their arthritis symptoms go into remission (their symptoms improve or completely disappear) during pregnancy. But that does not happen for every mother-to-be.
However, the pregnancy ‘glow’ that fills our newsfeed is a myth for many women, even without arthritis. Pregnancy can bring with it many unpleasant symptoms, which can be even more challenging if you have arthritis.
Pregnancy and arthritis remission
During pregnancy, your immune system goes through some changes to allow your baby to grow and develop.
For some women with arthritis, these changes to the immune system also bring a benefit of reducing the activity of their arthritis. It is thought that about half of women with rheumatoid arthritis will find that their symptoms, such as pain, stiffness and flares, improve during pregnancy.
However, there are many women with arthritis who continue to have active disease during their pregnancy. You may even find that your symptoms worsen, or you have disease flares, particularly if you’ve had to stop or change medications.
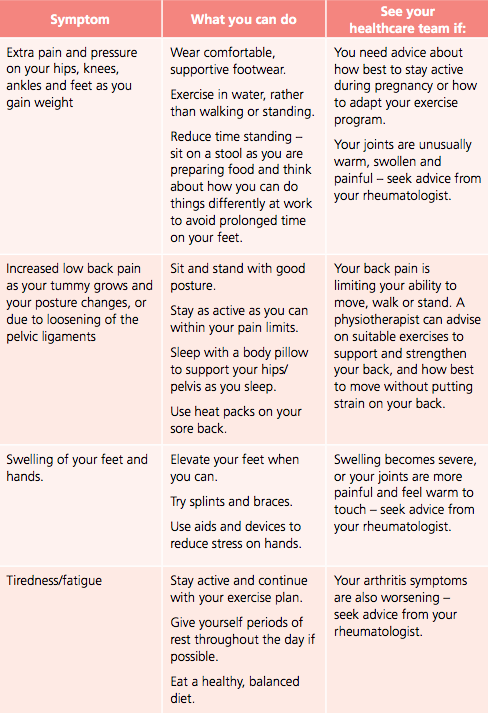
Physical effects of pregnancy
Pregnancy brings with it many physical changes to your body. If you are living with arthritis, some of these changes may even make your arthritis symptoms feel worse. Here are some common symptoms in pregnancy and tips for managing them:
Emotional health during pregnancy
Pregnancy can have a powerful effect on your mood, thoughts and emotions. Changes in your hormone levels can leave you feeling like you’re on an emotional rollercoaster at times, not to mention the impact of possible morning sickness, physical changes and bone-crushing tiredness. Some emotional ‘ups and downs’ are a normal part of pregnancy. However, if are feeling constantly sad, worried, scared or nervous, thinking negative thoughts about yourself, or are finding it difficult to sleep, eat or do the usual activities in your life, seek support.
Changes in your hormone levels can leave you feeling like you’re on an emotional rollercoaster at times
Talk to your GP or obstetrician about how you’re feeling, and they can suggest the best treatment options. You can also call the Perinatal Anxiety & Depression Australia (PANDA) National Helpline on 1300 726 306 for advice.
Labour and delivery
Throughout your pregnancy, you will no doubt hear many birth stories – some good, some bad and others you would rather not have heard! As these stories reveal, each birth is unique and rarely are they perfectly what the parents imagined.
Towards the end of your pregnancy, talk to your rheumatologist, obstetrician and/or midwife about how your arthritis could potentially impact on your delivery, such as:
- The positions you could use during labour and delivery. For example, there might be some positions that might be more comfortable if you have difficulties with your hips or lower back.
- Your ability to deliver your baby vaginally.
- The likelihood of requiring a caesarean section. Remember, while a caesarean section is more common in women with rheumatoid arthritis, many women without arthritis are also advised not to deliver their babies vaginally. A caesarean section may be the best option for a healthy baby.
- Your ability to have an epidural or spinal anaesthetic (pain relieving medications into the spine) during labour, especially if you have arthritis that affects your spine.
It is easy to get overwhelmed by the pressure to have a ‘normal’ vaginal birth. However, the most important goal at the end of your pregnancy is for both you and your baby to be healthy. Try not to get too preoccupied by the idea of a perfect birth. Instead, surround yourself with healthcare professionals who you trust, and keep your focus on that all-important end goal, a healthy, happy baby and mum.
Talk to your healthcare team about how your arthritis could potentially impact on your baby’s delivery.
Life with a new baby
The arrival of your tiny bundle of joy will undoubtedly change your life forever. Caring for a new baby is equal parts exciting and exhausting for all new parents. And, as a parent with arthritis, you may even experience some additional challenges.
Caring for a new baby
It is physically and emotionally demanding to care for a new baby, and even more so when you have arthritis either as a mum or dad. Here are a few tips that may help:
Nappy changing
- Have change stations set up in different parts of the house, with everything you may need to change your baby’s nappy, to make it easier if your mobility or ability to carry your baby is very limited.
- A change table on wheels may make it easy for you to move it around the house.
- Look for baby wipes and creams with easy to open lids.
- Ask someone to open the nappy packets for you or open them with scissors as they can be a challenge to get into with sore hands.
- Set up a change table that is at a height where you don’t need to bend over, or one where you can even sit while changing your baby’s nappy.
- While cloth nappies may be more environmentally friendly, disposables tend to be more absorbent, meaning you won’t need to change them as often. They will also save you a few extra loads of washing each week too. If using cloth nappies, look for ones with Velcro closures to make it quick and easy to change.
Bathing
- Look for baths that can be filled and drained in the sink or bathtub. Some baths come on trolleys that can be wheeled around.
- If you’re bathing your baby in a bathtub, look for supports or slings that they can lie on. Remember you will always need to closely supervise your baby in the bath.
- When your baby is very young, it might be easier to bathe him/her in the laundry trough/sink.
Cots, bassinets and highchairs
- Look for items that are easily height adjustable, lightweight and on wheels to make it easy to move them around the house.
- Test the clips, release mechanisms and brakes to ensure they are easy to use.
Dressing
- Look for clothing that is easy to put on and take off your baby, such as elastic waists and wide opening envelope necks. These will be easier on sore hands. Avoid snap closures, buttons and zips.
- Avoid socks and shoes for your baby if you have sore hands. Instead use jumpsuits that cover your baby’s feet.
Out and about
- Use a lightweight stroller or pram that is easy to fold, unfold and lift into your car. Test the harness to ensure it is easy to clip/unclip and adjust, and ensure the brakes are easy to use. Check the height of the handle and comfort for walking. A 15kg pram versus a 6kg pram may make all the difference. It’s worthwhile testing lots of different prams before you buy as sometimes the most expensive or popular ones are not necessarily the most user friendly.
- Use a pram caddy and baby bag to keep all your essentials close to hand when you are out. Try to keep your baby bag as light as possible. Consider using a backpack instead of a bag that sits on one shoulder or hang it off your pram.
- Try different baby carriers and slings to find one that can help you carry your baby without straining your hands, arms or shoulders.
Ask for, and accept, help
- Organise a network of supportive family and friends who can help you when you need it. This will be particularly important if you have a flare of your arthritis symptoms, or even just if you and your baby are having a bad day.
- New mothers without arthritis often need a support network too during the early months of life with a new baby.
- If you don’t have a support network of family and friends, investigate external help that may be available. Ask your obstetrician, midwife, community nurse or GP about support services that may be available in your area. Cleaners, nannies, au pairs, meal delivery services or other community-based supports in your area may be helpful.
- Make use of online shopping and home delivery services.
Listen to your body
- Pace yourself and be gentle with yourself. If you’re feeling exhausted, the house chores or tidying up can wait. Rest when your body is telling you it needs rest.
- Try to decide what tasks are a ‘must do’, what can wait and what can be outsourced to family, friends or hired help. Prioritise the tasks that absolutely need to get done as well as resting and enjoying your new baby. Don’t push yourself to get non-essential tasks done.
- Consider your own clothing; for example can you manage clips on maternity bras and tops, or is a pull down/up version easier?
Taking care of yourself
- It can be a huge adjustment in the first days, weeks and months with your new baby.
- Most women experience ‘the baby blues’ in the first days after your baby is born. This is very normal and may make you feel teary, irritable and overly sensitive. The baby blues usually go away after a few days.
- If you’re feeling low in mood and energy, having trouble sleeping or eating, feeling scared, sad, hopeless or angry for more than two weeks, seek help.
- You can talk to your GP, child health nurse, the Perinatal Anxiety and Depression (PANDA) Helpline (1300 726 306), your partner, friends and family. Getting the right support and treatment will help you manage post-natal depression and have you feeling better sooner.
Get advice from your healthcare team
- If you’re struggling to look after your baby because of pain or other symptoms, see your rheumatologist to talk about your treatment options.
- See a physiotherapist or occupational therapist for advice about looking after your joints and equipment that can make caring for your baby easier.
- Get advice from a child health nurse or lactation consultant for ways to make it easier to care for, and feed, your baby.
Breastfeeding and bottle feeding
Australian guidelines recommend exclusive breastfeeding for babies to around six months of age. Breastfeeding is then recommended to continue alongside suitable foods for infants until 12 months or age and beyond, for as long as the mother and child wish.
Whether to breastfeed or not, or for how long, is a very personal decision. Even mothers without arthritis can have issues that can prevent breastfeeding or make it very difficult.
There are usually no physical reasons that prevent women with arthritis from breastfeeding, apart from possible discomfort if you and your baby are not positioned correctly during feeding. You can get advice on this from your child health nurse or lactation consultant at your local hospital. The choice to either breast or bottle feed your baby will depend on many factors, such as your milk supply, your baby and the medications you are taking.
Breastfeeding and medications
Many arthritis medications are safe to take during breastfeeding as they do not pass into breast milk, or only in very low levels that are safe for the baby. Others can pass into your breast milk and will not be safe for your baby. Talk to your healthcare team, including your rheumatologist, about your plans for breastfeeding so that the best treatment plan, for both you and your baby, can be put into action when your baby is born.
See the table above for a summary of the safety of arthritis medications during breastfeeding.
Breastfeeding and joint pain
If you decide to breastfeed, here are some tips to make it more comfortable on your sore joints:
- Find a comfortable position. You might have a supportive chair at home already, or you might choose to invest in a breastfeeding chair, but make sure your neck and back are supported in a comfortable position. New babies feed all the time so make sure the chair is very comfortable as you will be spending a lot of your day (and night) in it. Some women find breastfeeding more comfortable lying on their side, so you may have to experiment with different positions before you find what works best for you.
- Breastfeeding pillows are a great way to support your baby, without putting strain on your hands, arms, shoulders and back.
- Seek advice from a lactation consultant or child health nurse if you are finding breastfeeding difficult or painful. They may be able to recommend a range of different equipment or aids that can make all the difference.
Bottle feeding and joint pain
Bottle feeding can also cause strain on sore arms, hands, necks and upper backs.
Here are some tips:
- Find a comfortable position. Make sure you sit in a comfortable chair that supports your neck and back. Use cushions or pillows to bring your baby to a height that’s comfortable for you to hold the bottle in their mouth.
- You could also try feeding your baby in a baby carrier, sling or rocker if it’s difficult holding your baby in your arms for long periods.
- Look for wider bottles that are more comfortable to hold in your hands.
- Ask your partner, family or friends who are visiting to help when they can.
- Consider asking for help if you can’t open the cans of formula or ask your partner to prepare the bottles if you’re going to be alone for a long period of time.
- Ask someone to help you with washing all the used bottles or use a steriliser or dishwasher to clean the bottles.
Post-natal flare
Just as you’re trying to cope with the sleep deprivation, and the physical and emotional demands of being a new mum, you might also have a flare of your arthritis symptoms.
Many women with arthritis find that their symptoms return or flare in the months after the baby is born. Post-natal flares are common, with studies suggesting up to 40% of women with rheumatoid arthritis experience a flare in the six months after giving birth.
This flare can make caring for your newborn very challenging. All the usual baby-care activities such as holding your baby during feeding, changing nappies, bathing, carrying and lifting your baby can be nearly impossible if you have severe joint pain and stiffness. You might also feel completely exhausted with arthritis-related fatigue on top of the sleep deprivation that comes with new babies.
It is a good idea to have an appointment booked with your rheumatology team four to six weeks after the birth.
If you notice your arthritis symptoms worsening in the weeks or months after the birth, get in touch with your rheumatologist straight away for advice about your treatment options and make an earlier appointment than planned.
A physiotherapist, occupational therapist or child health nurse may also be able to give you some practical advice about how to look after your baby during a flare. Using a baby carrier/sling and other equipment can make caring for your baby easier on your joints. See the section below for some tips about caring for a new baby when you have arthritis.
Most importantly, plan to get extra help. Have a support crew of family and friends on call for extra help if your arthritis flares. Don’t be afraid to ask for help from your network during this time when you might be struggling with even the most basic tasks.
Seeking support
Who can help?
Rheumatologists are doctors who specialise in diseases of the joints. Your doctor will need to refer you to a rheumatologist. They may recommend a rheumatologist or you can contact the Australian Rheumatology Association to find a rheumatologist.
A rheumatology nurse, if available, can help you understand your treatments, provide support and refer you to other health professionals.
A physiotherapist (physio) can use various treatments to keep your joints as flexible, strong and pain-free as possible. They will also show you exercises and pain-relief techniques to use at home.
An occupational therapist (OT) can provide advice on how to care for your baby without putting strain on your joints, including suggesting equipment and aids that can help.
Talk to your GP if you are finding your feelings and emotions are getting in the way of enjoying your life. They can suggest ways to cope, recommend medications that can help or refer you to a psychologist who can help you work through your feelings. You may be eligible for a Mental Health Care Plan, via your GP, which will provide subsidised sessions. You can also see a psychologist without needing a referral.
Perinatal Anxiety and Depression Australia (PANDA) supports women, men and families across Australia affected by anxiety and depression during pregnancy and early parenthood.
beyondblue provides information and advice about depression, anxiety, available treatments and where to get help.
Child health nurses are a wealth of information and support as you learn to care for your new baby. Ask your obstetrician or midwife or contact your local community health centre to find out about services in your area.
Lactation consultants can help you with any problems you might have with breastfeeding. Find out if your local hospital or child health clinic provides this service, otherwise you can pay for a private consultation.
The Australian Breastfeeding Association has a helpline 1800 mum 2 mum (686 268) and online forum to help you with any breastfeeding concerns.
The Independent Living Centre has information about aids and devices that can help with day-to-day activities.
Useful resources
The web can be a useful source of information and support. However, not everyone who puts information on the web is a qualified health practitioner. Some organisations make unrealistic promises in order to sell their products. Treatment options and practices from overseas may also not be relevant or approved in Australia. Always check information from the web with a trusted member of your healthcare team.
The Australian Government’s HealthInsite is an excellent starting point for web searches, as every site that HealthInsite links to has been checked for quality and accuracy of information.
Australian resources
Arthritis Australia’s website for people living with inflammatory arthritis www.empowered.org.au has a detailed section on pregnancy, including hearing directly from women with arthritis about their journeys to motherhood.
The Australian Rheumatology Association has a detailed document that outlines the most current evidence about the safety of arthritis medications during pregnancy.